Contents
What are sleep disorders?
Sleep disorder is a condition which affect good sleeping ability. Sleep is a biological process and quite complex in nature. During sleep, though we are unconscious, our brain and body functions are still active. They do a number of jobs to keep us healthy. Because of this, when we are sleep deprived, it not only makes us tired but hampers our daily functions and mental and physical health. There are different sleep disorders, some of which cause other underlying health conditions. We should identify sleep disorder symptoms and get proper treatment.
Sleep disorders are prevalent these days. In the U.S.A., 24% to 37% of school and college goers do not get adequate sleep. Stress, hectic work schedules etc., could affect our sleep. Still, when that sleep disturbance occurs regularly, it indicates a sleep disorder. One can have difficulty falling asleep, feel super tired, and have a low mood. Lack of concentration and health issues can occur depending on the types of sleep disorder.

Sleep disorders could also be because of some underlying medical conditions. One can find the sleep disorder’s reasons and treatment with the proper diagnosis. Once the real reason behind the disorder is found, appropriate medical treatment, therapy, or lifestyle changes could be made. The diagnosis and treatment should not be delayed for the sleep disorder. If not treated on time, the health consequences could be severe. It affects your health, relationships, work, school, and daily duties.
Recommended Sleep Times as per Age Group
Below chart shows the recommended sleep times for individual of different age groups.
| Age Range | Recommended Hours of Sleep | |
| Newborn | 0-3 months old | 14-17 hours |
| Infant | 4-11 months old | 12-15 hours |
| Toddler | 1-2 years old | 11-14 hours |
| Preschool | 3-5 years old | 10-13 hours |
| School-age | 6-13 years old | 9-11 hours |
| Teen | 14-17 years old | 8-10 hours |
| Young Adult | 18-25 years old | 7-9 hours |
| Adult | 26-64 years old | 7-9 hours |
| Older Adult | 65 or more years old | 7-8 hours |
Apart from age, certain other factors affect how much sleep one needs.
Sleep quality. Good quality of sleep is essential. If it is interrupted continuously, you will lack vital energy for your daily activities.
Previous sleep deprivation. The amount of sleep needed increases if one is also sleep deprived.
Pregnancy. During pregnancy, the changes in hormone levels and physical discomfort results in poor quality of sleep.
Ageing. Older adults need a good amount of sleep, just like an adult. But with age, sleep patterns change. They tend to have a lighter sleep and sleep for a shorter duration. Older adults are also prone to wake up at night many a time.
The recommended amount of sleep helps kids to have better health. It also improves their behaviour, memory, emotions, attention to tasks etc.
Suppose adults do not get adequate or at least 7 hours of good sleep. In that case, physical and mental health-related problems such as depression, anxiety, high blood pressure, heart disease, and diabetes appear.
Types of Sleep Disorder
There are many types of sleep disorders. Let’s check one by one.
1. Insomnia

It is referred to as insomnia when someone cannot fall asleep or stay asleep. There are various reasons for insomnia like stress, anxiety, hormonal changes, health problems, jet lags etc. Insomnia can create a problem as it can cause
- Depression
- Irritability
- Lack of concentration
- Difficulty in weight management
Insomnia is prevalent among older adults and women. It could be divided into 3 types.
- When insomnia happens regularly for 1 month at least, it is called chronic insomnia.
- If it happens periodically, then it is termed intermittent insomnia
- It is called transient insomnia, which lasts for just a few nights.
2. Sleep Apnea
Sleep apnea is a severe medical condition. The main characteristics of sleep apnea are pauses in breathing during sleep and waking up during the night due to less oxygen in the body.
It is generally of two types.
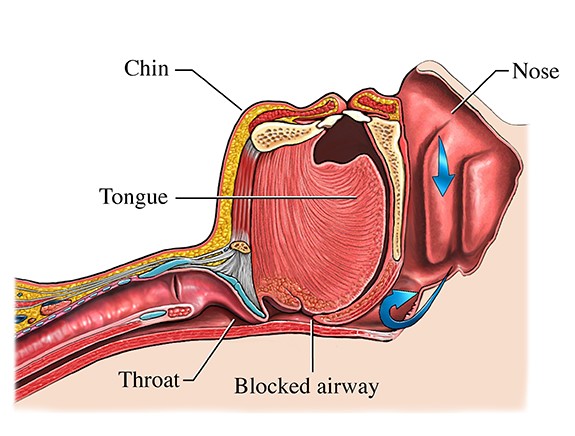
Obstructive Sleep Apnea (OSA)
In obstructive sleep apnea, the airflow is hindered due to obstruction in the airway or too narrow an airway. Soft tissues in our throat relax during sleep, and these tissues can block the upper airway. Once the airway is blocked, the body’s oxygen levels drop, and the person wakes up to breathe normally again.
The waking up session could be for a few seconds only, and the person with OSA might not be aware of being awake. Severe sleep apnea may cause someone to wake up hundreds of times during sleep, interrupting the sleep cycle. This can cause daytime fatigue and sleepiness.
Central Sleep Apnea (CSA)
In central sleep apnea, the brain and muscles that control breathing suffer from connection problems. It happens because the brain does not tell our body to breathe. As a result, hypoventilation/hypoxemia can be caused. It is different from obstructive sleep apnea as, in this case, there is no effort to breathe as there is no urge to breathe.
3. Parasomnia
Parasomnias are sleep disorders responsible for abnormal movements and behaviour during sleep. The activity and behaviour include
Sleepwalking/Talking
It is also known as Somnambulism. In sleepwalking, the person behaves as being awake, appears to be awake but is actually sleeping. In the case of sleep talking, the person vocalizes in their sleep. It could be a few words or a complete conversation. The person generally has little to no memory of the event. It may involve routine activities like walking to the bathroom, getting in a car, or driving. Somnambulism can occur at any age but is prevalent in children. It often goes away as the child grows older. Excessive fatigue, stress, anxiety, illness etc., can cause sleepwalking.
Sleep Terrors
Sleep terrors are also called “night terrors”. There are episodes of extreme terror and a temporary inability to attain full consciousness. The person could display behaviours such as fear, panic, confusion, etc. They may experience gasping, moaning or screaming. However, the person is not fully awake. Once the episode passes, the person often returns to normal sleep without completely waking up. Mostly, there is no recollection of the attack in the morning.
Sleep terror usually occurs during slow-wave sleep. They primarily happen during the first part of the night, while nightmares occur during the last third of the sleep period. The timing of the events helps to differentiate sleep terror from nightmares.
Though sleep terrors are more common in children but can occur at any age. Research indicates that night terror could be a hereditary problem. Stress, fatigue or any irregular routine triggers sleep terror.
Confusional Arousals
In confusional arousal, a sleeping person appears to be awake, but their behaviour is unusual or strange. The individual could show symptoms like disorientation, unresponsiveness, speech issues etc. The state may last a few minutes or can continue for an extended period. It usually lacks recall of the arousal or any event that may have occurred during the episode the following day.
Sleep Paralysis
Sleep paralysis is considered a disorder outside of REM sleep. It can occur in healthy people and those presenting symptoms of narcolepsy, cataplexy and hypnagogic hallucinations. When it happens without narcolepsy, it is classified as Isolated Sleep Paralysis (ISP).
Muscle atonia or sleep paralysis occurs when a person falls asleep or awakens. If one has awareness while the body enters or exits REM sleep, they may experience sleep paralysis. Vivid hallucinations can happen during sleep paralysis. Excessive stress, alcohol consumption, sleep deprivation, and narcolepsy can cause sleep paralysis.
Nightmares

Nightmares are vivid dreams containing frightening images that cause fear, terror, and extreme anxiety. If one is awakened from REM sleep during a nightmare, they can provide a detailed description of the dream. The nightmare causes the sufferer distress, sweating and an increased heart rate.
It takes some time to recover from a nightmare, and the negative emotions and the person may have difficulty going back to sleep. Nightmares generally occur during the last third of the night.
Anxiety, illness or an uncomfortable position can lead to bad dreams. Post-traumatic stress disorder can trigger frequent nightmares, as can side effects from medications and narcotics such as amphetamines and cocaine.
Several medical and non-medical methods alleviate the conditions that often cause chronic nightmares. Solving stress in the home or personal life will often reduce bedtime anxiety. Regular exercise, yoga and meditation help to reduce stress and improve sleep quality.
Rapid eye movement (REM) sleep behaviour disorder
Normal sleep can be divided into two stages non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. People generally do not move during REM sleep, which comprises 20% of our total sleep. It is a time when we usually dream.
Rapid eye movement (REM) sleep behaviour disorder occurs when one acts out vivid and unpleasant dreams with vocal sounds and body movements. Vocal sounds like talking or yelling and physical body movements like punching, kicking or sitting etc., are also known as dream-enacting behaviour. The onset of REM sleep behaviour disorder is often gradual and can worsen with time.
The person may be awakened or wake spontaneously during the attack and vividly recall the dream that corresponds to the physical activity.
4. Restless Leg Syndrome
In the case of restless leg syndrome (RLS), one feels the urge to move the legs during sleep. Research suggests low brain iron metabolism could be a critical pathway in the pathophysiology of RLS. In RLS patients, blood ferritin levels are low. Iron deficiency is also pronounced when measured in the brain or Cerebrospinal fluid (CSF). Dopamine is an important neurochemical in our brain. Its abnormal level can also be a reason behind RLS.
Genetic factors are strong predictors of RLS as RLS commonly runs in the family. DNA changes in five genes, MEIS1, BTBD9, MAP2K5/LBXCOR1, and PTPRD, could also be the reason behind restless leg syndrome.
5. Narcolepsy
In narcolepsy, one feels extremely tired suddenly and then falls asleep. It can also cause sleep paralysis, and one can even move after waking up. It is a chronic sleep disorder which can cause excessive daytime sleepiness (EDS). The exact reason behind narcolepsy is not fully understood, but it is often associated with neurological disorders and genetic factors. Narcolepsy causes sudden sleep attacks and sudden loss of muscle tone and can cause hallucinations.
What are the sleep disorder symptoms?
Sleep disorder symptoms depend on the type of disorder, its severity and if it results from any underlying medical conditions.

Common symptoms are
- Difficulty in falling asleep
- Sleep disorder symptoms could be difficulty in staying asleep
- Unusual breathing troubles
- Urge to move while sleeping
- Changes in sleeping and waking schedule
- Fatigue
- strong desire to sleep during the day
- Irritability
- Anxiety
- Poor performance at work or school
- Lack of concentration may be one of the Sleep disorder symptoms
- Depression
- Weight gain or loss can be one amongst many Sleep disorder symptoms
What causes sleep disorders?
There are many conditions or illnesses which can cause sleep disorders. The underlying disease is one of the significant causes behind it. As a result of sleep disorders, our body’s natural sleep cycle gets disturbed. Below are a few reasons behind the disorder.
Mental Issues: Stress, anxiety, and depression are significant contributing factors which harm our sleep quality. They make it difficult to fall asleep or stay asleep.
Physical disturbances: Physical disturbances such as arthritis, chronic fatigue syndrome, fibromyalgia, inflammatory bowel disease, persistent headaches, and continuous lower back pain can cause the disorder.
Medical issues: Medical issues like sleep apnea cause sleep disorders.
Environmental issues: Bright light, outside noise, snoring.

Genetics: Disorders like narcolepsy has a strong connection with human or, rather say, family genetics.
Night shift work: People who do night shifts often experience sleep disorders as their activities run against their body’s biological clock.
Medications: Medication such as antidepressants, blood pressure medication, and over-the-counter cold medicine can interfere with sleep.
Ageing: Persons over 65 have a sleep disorder. It is unclear whether it is a normal part of ageing or a result of medications that older people use.
Allergies and respiratory problems
Upper respiratory infections, cold, blocked nose and allergies make breathing challenging at night.
Frequent urination
Imbalances in our hormones or diseases of the urinary tract may contribute to the development of nocturia. It is a frequent urination illness and can disrupt sleep by causing one to wake up at night.
How to diagnose sleep disorders?
The healthcare professional gathers information from sleep disorder symptoms, medical history and physical tests. Some tests could be performed, such as
Polysomnography (PSG): Polysomnography gathers information on brain waves, blood oxygen levels, heart rate, breathing rate and body movements. It is a comprehensive test to diagnose sleep apnea, insomnia, and restless leg syndrome. One must spend a night at a sleep laboratory in a hospital or an outpatient sleep clinic.
Electroencephalogram (EEG): Electroencephalogram records electrical activity in the brain using small metal discs (electrodes) attached to the scalp. Our brain cells communicate through electrical impulses, which are always active, even when asleep. These electric impulses show up as wavy lines on an EEG recording. It is used to find out about sleep disorders and many brain disorders.
Multiple sleep latency tests (MSLT): How quickly a person falls asleep is called sleep latency. This daytime napping study uses a PSG at night to help diagnose narcolepsy. Multiple sleep latency tests give a person 4 to 5 opportunities to sleep after every two hours during regular wake times. The data is used to determine the extent of daytime sleepiness and how fast REM sleep begins.
These tests are significant for determining sleep disorders and the proper treatment.
How to treat sleep disorders?
The type of sleep disorder and the underlying cause of the illness determines the treatment. In general, doctors use medical treatments and suggest lifestyle changes for the treatment.
Medical treatments
- Sleep medicines.
- Medication for allergy or cold.
- Medications for underlying health conditions.
- Breathing device or surgery for disorders like sleep apnea.
- A dental guard for teeth grinding.
- Cognitive behavioural therapy or relaxation techniques.
- Using continuous positive airway pressure machine or CPAP machine to treat sleep apnea.
- Bright light therapy in the morning.
Lifestyle changes
Changes in our lifestyle significantly improve sleep quality.
- There should be plenty of vegetables and animal protein in our diet. Also, sugar intake should be reduced.
- Regular exercise reduces anxiety and stress and enhances sleep quality.
- A regular sleeping schedule is essential to improve sleep quality. One should not divert from the plan even at the weekend.
- Drinking less water before bedtime can help avoid frequent urination at night and hampers sleep.
- There should be a limit on caffeine intake in the later part of the day.
- Reduce usage of tobacco and alcohol.
- Weight management.
- Minimize noise and light.
References
- Key sleep disorders. (2019, February 13). Cdc.gov.
- Kristen, H. A. (2018). Pediatric sleep disorders. In Sleep Disorders and Sleep Promotion in Nursing Practice. Springer Publishing Company.
- Understanding sleep disorders. (n.d.). Ohsu.edu. Retrieved August 3, 2022
